Please note that this post contains descriptions of anxiety, depression, and suicidal ideation. I ask that you read with caution if these are difficult topics for you. Thanks for being here.
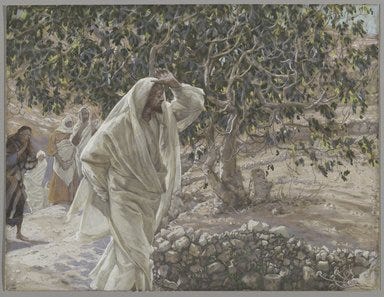
The Accursed Fig Tree, James Tissot
What am I doing wrong, God? What am I doing wrong?
It was 2:41 a.m. and I was on the floor of our half-bathroom, eyes burning with angry tears and the desperate ache to sleep.
It was my fifth night in a week with insomnia—a week that included my son and I contracting Covid, my daughter going back to school, and my husband working two nights at the stadium until after two a.m.—and I was running on fumes. I’d slept a total of no more than nine hours in about five days and I was spiraling. Heart racing with anxiety each night, I would tuck myself into bed with dread pulsing through my body. My pillow had become a terror, my comforter a prison guard. Cortisol bloomed hot in my chest and spread out into my limbs like wildfire, destroying my parasympathetic nerves.
Finally, I had a panic attack.
My husband was so gracious and gentle with me, as he always is, but it didn’t matter. My brain could not shut off and my fight or flight response had taken over. I wanted to die. I wanted to crawl out of my body. I wanted to fucking sleep.
What am I doing wrong, Lord?
I’ve touched on my difficulties with sleep in the past. For most of my life, rest was never a problem. I could sleep almost anywhere as long as I could get supine. But after a traumatic experience with the malaria medication Mefloquine in 2011 which put me on a ten-day anxiety spiral while thousands of miles away from my family—resulting in almost no sleep for more than a week, terrifying harm thoughts, and my first brush with suicidal ideation—I now find sleeping anywhere but in my own home with my own family a great challenge. Vacations, weekends away, sleeping over with extended family…all of it now induces some sort of sleep anxiety to varying degrees. Which, in short, sucks ass.
A lot of my sleep anxiety has to do with Mefloquine. I never experienced it before taking that (VERY-DANGEROUS-0/10-DO-NOT-RECOMMEND) drug. It has known neurological side effects that can cause permanent damage, especially for people already living with a mental health disorder—which I didn’t know until years after it was out of my system. (Thank you, Dekalb County Public Health Department.) The other part of my sleep anxiety is O.C.D. Once my brain has settled on a thought—like how I really, really want to go to sleep—trying to release that thought looks a bit like this:
Thus, the anxiety about sleeping increases, which causes more sleeplessness and more anxiety.
The treatment, of course, is to care for myself the same way I do with any other obsession: with cognitive behavioral therapy, or CBT. Anything I do to “try” to get to sleep is considered a “sleep effort” and such behavior only reinforces those neural pathways telling me I won’t sleep. (Sleep hygiene only works so well here. It’s not about the coffee; it’s about my brain.) I must look at those fears, acknowledge them, and tell myself a truer story.
I don’t have to try to sleep. I can simply go to bed when I’m sleepy. My body knows what to do. If I can’t sleep, I’ll get up and do something gentle that I enjoy. I will probably be tired tomorrow, but that’s alright. Sometimes, life is hard. And that’s okay, too.
Following two psychiatric appointments and a couple of new meds, I finally slept like a baby. Still, the anxiety remained during the day because I was anticipating the night when I would stop taking the primary sleep med, which is a benzodiazepine and obviously not for long-term use. (I’d only been prescribed seven days worth of it.) On my doctor’s orders, I’d already begun to taper it every other night by taking a quarter less, and it was still effective for a good night’s sleep.
In my waking hours, though, I could feel the constant, low-grade hum of what if in my belly.